Thymus surgeon in North India
Body
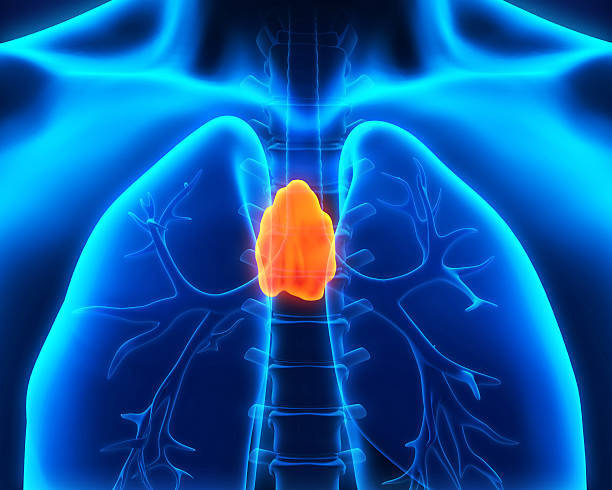
The thymus gland is in the front part of the chest just behind the breast bone and in front of the heart, an area known as the anterior mediastinum, with parts (lobes) extending into the neck. The thymus is part of the body’s immune system, and plays its largest role early in a person’s development. Surgical removal of the thymus has no effect on the immune system for someone after they are born.
A thymectomy is the surgical removal of the thymus gland, which has been shown to play a role in the development of myasthenia gravis. Roughly 10 percent of patients with myasthenia gravis have a thymoma, or a tumor on the thymus gland. While most of these slow-growing tumors are benign, some may be cancerous (malignant).
A thymectomy is recommended for patients under the age of 60 years who have moderate to severe weakness from myasthenia gravis. It may be recommended for patients with mild weakness if it impacts breathing or swallowing. The procedure is also recommended for anyone with a thymoma.
Benefits
In patients for whom a thymectomy is recommended, there can be several treatment goals, including:
- Reducing patient weakness
- Reducing the use of medications
- Achieving permanent remission of the disease
- Thymus surgeon in North India
Thymectomy is considered a means of helping a patient improve their condition in the long term.
Surgery
There are three main surgical approaches for thymectomy:
- Trans-sternal: This anterior (frontal) approach goes through the sternum, removing the thymus and, as necessary, the fat next to the thymus. Some approaches may include the neck to ensure removal of all of the thymus.
- Transcervical: This anterior transverse (horizontal) approach is by means of the lower neck and may involve the chest to remove fat adjacent to the thymus.
- Videoscopic (VATS): This approach uses small incisions in the chest (right or left side) and thin, flexible tubes (scopes) with fiber optics to let the surgeon see and remove the thymus and, as necessary, adjoining fatty tissue.
- Thymus surgeon in North India
The trans-sternal approach is the most often used approach for removal of a thymoma.
While the surgical approaches vary, the goal remains the removal of as much of the thymus as possible for best possible outcome. Some surgeons advocate the removal of the fatty tissue adjoining the thymus, while others feel the removal of the thymus alone is sufficient.
The extended form of trans-sternal thymectomy, with the removal of the adjoining fatty tissue, is the most frequently used approach, while the proponents of the transcervical and VATS minimally invasive approaches believe theirs are as effective.
Discuss these surgical approaches with your physician to determine which is right for you.
Recovery
Depending on the type of surgery and on the condition of the patient, a ventilator may be required after surgery. Once the breathing tube has been removed, the patient will be asked to breathe deeply and cough repeatedly to clear the lungs of mucus.
The patient may have one or two chest tubes (small tubes in the chest attached to drainage bottles), which will be removed shortly after surgery.
Pain levels are mild after transcervical or VATS thymectomies. There can be more pain with the trans-sternal approach, but it is temporary and can be controlled through use of pain medications. Pain usually resolves in three to five days.
Your length of stay in the hospital depends on the surgical approach used and your overall strength. Most patients are able to be discharged in a few days to a week.
Time away from work and other activities depends on your condition, the type of surgery you received and the nature of your work. On average, limiting activities for three to six weeks is common, with longer time before more strenuous jobs and activities can be considered.










Comments